What Is Occipital Neuralgia?
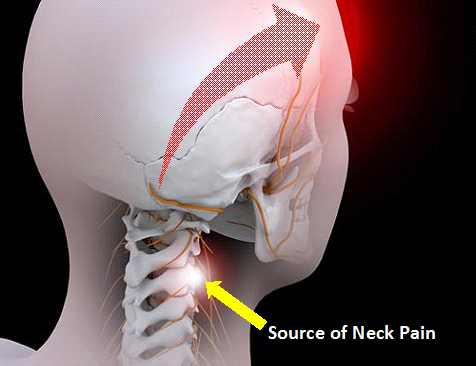
A headache is not always just a headache. Most people have heard of migraine headaches, tension-type headaches, and cluster headaches. But many may not have heard of Occipital Neuralgia. Sources of pain in the upper cervical spine-like the ligaments, joints, muscles and nerves can result in occipital neuralgia.
A 44 year old woman, Mrs Chan, always comes home from work with a headache which usually starts around mid-afternoon period. She is a secretary in a bank and works long hours in front of the computer; but this headache was different than the migraines she was used to getting. This new headache is always on the left side and seemed to come from the base of her skull and spread towards the top of her head. Whenever she spends long periods of time working on the computer, the headache gets worse.
What Causes Occipital Neuralgia?
Simply undergoing an excessive amount of stress to your neck and spine is itself a cause of Occipital Neuralgia.There are several other factors that can make Occipital Neuralgia more severe or happen more frequently. These include fatigue, problems sleeping, disc problems (the intervertebral discs between the bones in your neck can “slip” backwards), previous neck injuries, poor posture and muscular strain.
Occipital Neuralgia is usually one sided (although can be on both sides if neck pain also equally bad on both sides); it starts from the neck and then spreads to the back, side and often also to the front of the head. The headache initially begins in episodes and then slowly progresses to an almost continuous pain.
Unlike migraines, Occipital Neuralgia usually starts during the middle-age years and tend to get worse as one gets older. In contrast to tension-type headaches, Occipital Neuralgias usually one-sided, rarely crossing the midline. Most importantly, Occipital Neuralgia tends to get worse with certain neck postures or movements. Cervical postures and movements that provoke head pain are a primary diagnostic clue for classifying Occipital Neuralgia. Using the cited example, the secretary is often working at her computer when the headaches start. If a computer screen is too high, she is forced to look up for prolonged periods of time. This neck extension can lead to cervical facet joint strain and in due process result in headaches originating from the cervical spine.
When the upper cervical spine joints start hurting, the upper cervical nerves usually react soon after. Unfortunately, the upper cervical nerves intricately interact and converge with the Trigeminal Nerve (a cranial nerve). As a result, headaches start from the back of the head, radiates to the forehead and can be associated with facial and jaw pain. The head and the neck are closely intertwined in many ways and that relationship is what leads to the Occipital Neuralgia. As the cervical musculoskeletal system is linked directly to the head, treatment of Occipital Neuralgia needs to address the problem in the neck. Ultimately, the specific classification of headaches like Occipital Neuralgia leads to better treatment because a headache is not just a headache.
During the consultation, I noticed Mrs Chan’s inability to turn her head fully due to pain. It was also obvious that there was a lack of side-bending range of motion in the cervical spine. An X-Ray suggested the presence of arthritic joints in the cervical spine. After carefully considering the entire history and exam, it appeared that Mrs Chan is suffering from Occipital Neuralgia.
How Is It Diagnosed And Treated?
Common symptoms ofOccipital Neuralgia include a steady, non-throbbing pain at the back of the head, towards the base of the skull. This is often associated with neck pain which may also spread to between the shoulder blades. The pain can also spread to the forehead and is often worse on one side of the head. Pain is usually made worse by sudden neck movements, such as a sneeze. Along with head and neck pain, accompanying symptoms may include nausea, vomiting, dizziness, blurred vision, and feeling pain travelling down one or both arms. The neck is often very stiff and the patient may have trouble turning his head at times during painful episodes.
The diagnosis of Occipital Neuralgia begins with a careful history taking and physical examination and followed by appropriate diagnostic studies that includes cervical spine X-rays, MRI, electromyography; and diagnostic nerve blocks which may also be used to confirm the diagnosis.
Initial management of Occipital Neuralgia usually starts with simple analgesics, such as NSAIDs and Paracetamol. Physiotherapy is also started early in order to reduce loss of range of motion in the neck. However, treatment of Occipital Neuralgias should in fact focus on the source of pain in the cervical spine. Minimally invasive procedures that target these sources include trigger point injections, greater or lesser occipital nerve blocks, facet joint blocks, diagnostic nerve root blocks, and discography. The choice of procedures will ultimately depend on what is diagnosed as the main source of the Occipital Neuralgia in the individual patient.
Can It Be Prevented?
There is no direct and identified prevention measures that could help a person avoid the onset or development of Occipital Neuralgias. However, good ergonomics and proper neck posture may reduce the stress on the neck joints. In addition, healthy diets, sufficient sleep and reduced overall tension and stress is always recommended.
Dr Nicholas HL Chua, Ph.D
MBBS MMed (Anaes) FIPP (WIP) Dipl.AAPM FAMS (Anaes)
MEDICAL DIRECTOR, SPECIALIST PAIN INTERNATIONAL CLINIC
#12-03 MT ELIZABETH MEDICAL CENTRE
#07-22/23 Mt Elizabeth Novena Specialist Medical Centre
